1
INCOMPETENT TO STAND TRIAL
SOLUTIONS WORKGROUP
Report of Recommended Solutions
A report of recommended solutions presented to the California Health
and Human Services Agency and the California Department of
Finance in Accordance with Section 4147 of the Welfare and
Institutions Code
N
ovember 2021
2
TABLE OF CONTENTS
I. Purpose of the Workgroup and Report ………………………..
3
II. Incompetent to Stand Trial Crisis – a History ………………
5
a. The IST Process ……………………………………………..
5
b. National Data and California Data …………………………
6
c. Individual Patient Characteristics .………………………...
9
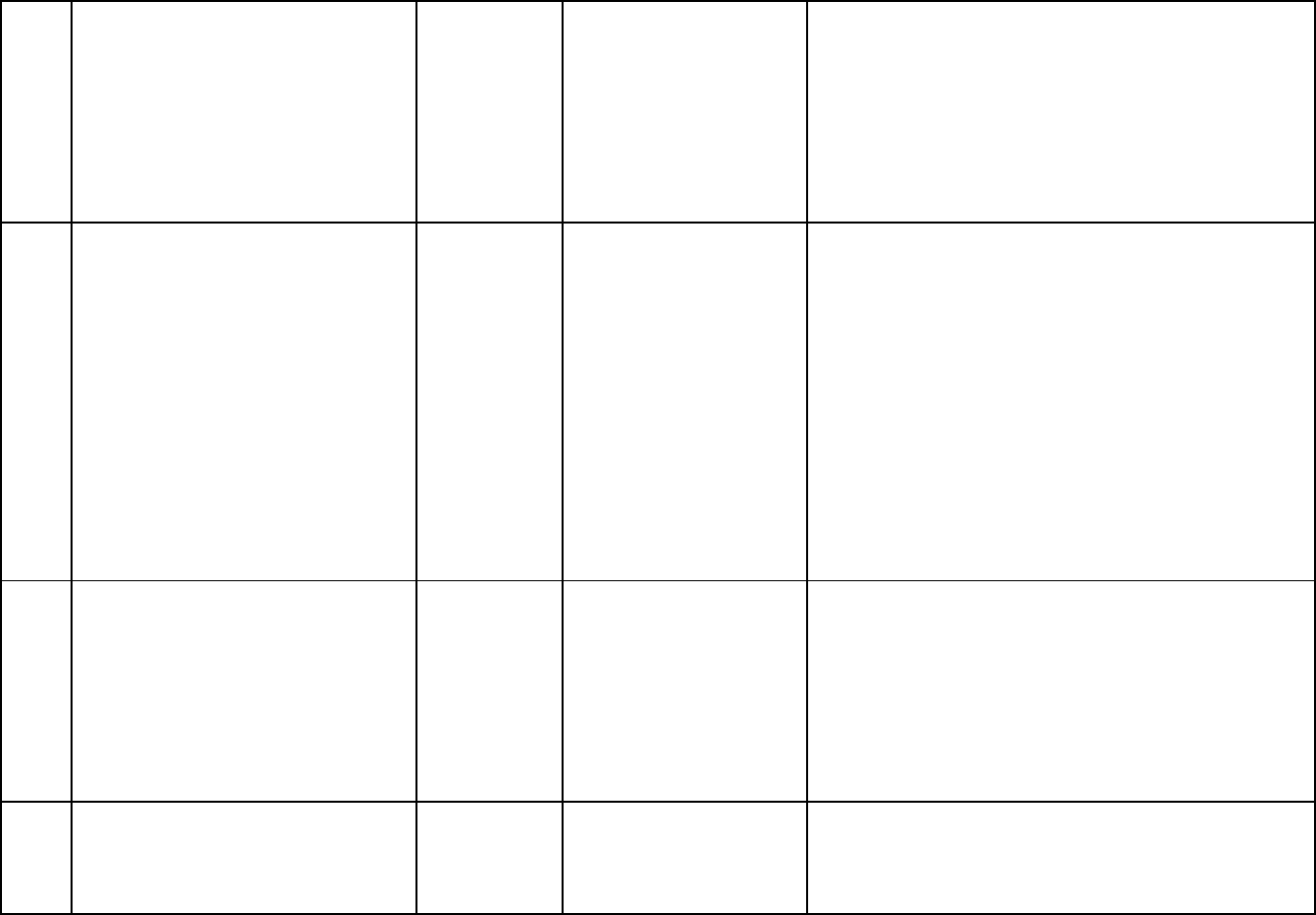
III. Department of State Hospitals Efforts to Date ………………
11
a. Increased Capacity at DSH ………………………………
11
b. Systems Improvement ……………………………………..
15
c. Demand ………………………………………………………
17
IV. IST Solutions Workgroup Process …………………………….
19
a. Guiding Principles for Generating Recommendations .…
20
b. Process for Synthesizing Recommendations ……………
21
V. Census of Recommended Solutions from the IST
Workgroup Meetings for Submission to CalHHS and DOF ...
22
a. Short Term Strategies: Solutions that can begin
implementation by April 1, 2022 ……………………………
22
b. Medium-Term Strategies: Solutions that can begin
implementation by January 10, 2023 ……………………...
31
c. Long-Term Strategies: Solutions that can begin
implementation by January 10, 2024 and
January 10, 2025 …………………………………………….
50
VI. Appendix A: IST Solutions Working Group Membership and
Affiliations ……………………………………………………….
65
3
I. Purpose of Workgroup and Report
The Legislature enacted Welfare & Institutions Code (WIC) section 4147 through the
passage of Assembly Bill 133 (Chapter 143, Statutes of 2021) and the Budget Act of
2021 (Chapter 69, Statutes of 2021), which charged the California Health & Human
Services Agency (CalHHS) and the Department of State Hospitals (DSH) to convene an
Incompetent to Stand Trial Solutions (IST) Workgroup (Workgroup) to identify
actionable solutions that address the increasing number of individuals with serious
mental illness who become justice-involved and deemed Incompetent to Stand Trial
(IST) on felony charges.
The purpose of the Workgroup is to identify solutions to advance alternatives to
placement in DSH restoration of competency programs and includes strategies for
reducing the number of individuals found incompetent to stand trial; reducing lengths of
stay for felony IST patients; providing early access to treatment prior to transfer to a
DSH program; and increasing diversion opportunities and treatment options, among
other solutions. Per WIC Section 4147, the Workgroup must submit recommendations
to CalHHS and the Department of Finance on or before November 30, 2021, for short-
term, medium-term, and long-term solutions that provide timely access to treatment for
individuals found IST on felony charges. The IST Workgroup convened between August
2021 and November 2021 and held five meetings and nine topic-focused sub-working
group meetings with a number of representatives and stakeholders from several state
agencies, the Judicial Council, local government and criminal justice system
representatives, and representatives of IST patients and their family members.
This report describes: 1) the background of the increasing numbers of referrals of
individuals committed as IST in California and across the nation, 2) an overview of the
IST Workgroup and the process utilized to develop the recommended solutions, and 3)
a census of recommendations provided by the members of IST Workgroup and
stakeholders to the CalHHS and Department of Finance.
The census of recommendations provided in Section V represents the gathering of the
collective discussion and recommendations from members of the IST Solutions
Workgroup and sub-working groups and input from public participation in the meetings
of these groups. Consistent with the direction provided by statute, any
recommendations that did not represent actionable short, medium, or long-term
solutions are not included. These recommendations do not represent the viewpoints or
opinions of any one entity or the State, nor do they represent consensus of the
members of IST Solutions Workgroup. Some IST Solutions Workgroup members may
support or oppose specific recommendations. All recommendations received by the
Workgroup, meeting minutes and specific support, opposition, and feedback by
individual IST Solutions Workgroup members and the public may be found at the IST
Solutions Workgroup website:

4
• https://www.chhs.ca.gov/home/committees/ist-solutions-workgroup/
IST Solutions Workgroup Members and their affiliations:
• Chair: Stephanie Clendenin, Director, California Department of State
Hospitals (DSH)
• Stephanie Welch, Deputy Secretary of Behavioral Health, California Health and
Human Services Agency
• Nancy Bargmann, Director, California Department of Developmental Services
o On occasion Director Bargmann was represented by Carla Castaneda,
Chief Deputy Director of Operations, California Department of
Developmental Services; and Dawn Percy, Deputy Director, Department
of Developmental Services
• Adam Dorsey, Program Budget Manager, California Department of Finance
• Brenda Grealish, Executive Officer, Council on Criminal Justice and Behavioral
Health, California Department of Corrections and Rehabilitation, Office of the
Secretary
o On occasion, Executive Officer Grealish was represented by Monica
Campos, Council on Criminal Justice and Behavioral Health, California
Department of Corrections and Rehabilitation, Office of the Secretary
• Tyler Sadwith, Assistant Deputy Director, Behavioral Health, California
Department of Health Care Services
o On occasion Assistant Deputy Director Sadwith was represented by Jim
Kooler, Deputy Assistant Director, California Department of Health Care
Services; and Elise Devecchio-Cavagnaro, Consulting Psychologist,
California Department of Health Care Services
• Brandon Barnes, Sheriff, Sutter County Sheriff’s Office
o On occasion Sheriff Barnes was represented by Cory Salzillo, Legislative
Director, California State Sherriff’s Association
• John Keene, Chief Probation Officer, San Mateo County & President-Elect,
Chief Probation Officers of California
• Stephanie Regular, Assistant Public Defender, Contra Costa County Public
Defender Office & Co-Chair of the Mental Health Committee of the California
Public Defender Association
• Veronica Kelley, Director, San Bernardino County Department of Behavioral
Health & Board President, California Behavioral Health Directors Association
o On occasion, Director Kelley was represented by Michelle Cabrera,
Executive Director, California Behavioral Health Directors Association
(CBHDA)
• Farrah McDaid Ting, Senior Legislative Representative, Administration of
Justice, California State Association of Counties (CSAC)
o On occasion Josh Gauger, Legislative Representative, California State
Association of Counties (CSAC) also represented CSAC
• https://www.chhs.ca.gov/home/committees/ist-solutions-workgroup/
5
• Scarlet Hughes, Executive Director, California Association of Public
Administrators, Public Guardians and Public Conservators
• Jessica Cruz, Executive Director, National Alliance of Mental Illness – California
• Pamila Lew, Senior Attorney, Disability Rights California
o On occasion, Kim Pederson, Senior Attorney, represented Disability
Rights California
• Francine Byrne, Judicial Council of California
• Jonathan Raven, Chief Deputy District Attorney, Yolo County
II. Incompetent to Stand Trial Crisis – a History
Overview
Over the last decade, the State of California has seen significant year-over-year growth
in the number of individuals charged with a felony offense who are found Incompetent to
Stand Trial (IST) and committed to the State Department of State Hospitals (DSH) for
competency restoration services. The State of California has responded to the
substantial growth in the felony IST population through multiple investments to increase
DSH’s capacity to serve these individuals with serious mental illness. However, the
growth in the felony IST patients has exceeded the capacity and outpaced other efforts
to respond to the growth in the felony IST population, resulting in growing waitlist and
wait times to admission. In 2015, the American Civil Liberties Union sued DSH
(Stiavetti v. Ahlin
1
) regarding the amount of time IST defendants were waiting for
admission into a DSH treatment program alleging violations of individuals’ due process
rights. The Alameda Superior Court ultimately ruled that DSH must commence
substantive treatment services in 28 days for felony IST patients. DSH appealed this
ruling and ultimately in the summer of 2021, the Superior Court’s order was affirmed.
Meanwhile, the worldwide COVID-19 pandemic has significantly exacerbated DSH’s
ability to meet the IST demands and as of November 2021 over 1,700 individuals are
awaiting restoration of competency treatment.
The IST Process
IST defendants are determined by a court to be unable to participate in their trial
because they are not able to understand the nature of the criminal proceedings or assist
counsel in the conduct of their defense. When the court finds a felony defendant
incompetent to stand trial in California, they can be committed to DSH to provide clinical
and medical services with the goal of restoring their competency and enabling them to
return to court to resume their criminal proceedings.
As court proceedings in a defendant’s trial are beginning, the defense attorney may
raise a doubt with the court that the defendant may be incompetent (doubt can also be
1
As of 12/01/2021 this case will be renamed Stiavetti v. Clendenin

6
raised by the prosecution and by the court itself). Once a doubt is declared, the court
will order an independent evaluation of the defendant by a court-appointed psychiatrist
or psychologist (also known as an Alienist). If the alienist finds that the individual is
incompetent, the court defers the current legal proceedings and orders a placement
evaluation by the CONREP Community Program Director to determine if the felony IST
should be treated in a DSH inpatient facility or an outpatient program.
The focus of treatment for the IST population is on restoration of trial competency in the
most expeditious manner so that the deferred legal proceedings can resume, not to
establish long-term mental health treatment for an individual. To this end, the training of
criminal procedures is continuously the focus of the treatment milieu for IST
patients. Once specific mental health issues and medication needs are addressed,
patients are immersed in groups or individualized sessions that train them in various
aspects of court proceedings. Each patient receives instruction as to what they are
charged with, the pleas available, the elements of a plea bargain, the roles of the
officers of the court, the role of evidence in a trial, and their constitutional
protections. Knowledge of these areas is assessed using a competency assessment
instrument. Additionally, an IST patient may participate in a mock trial where staff
members act as judge, jury, district attorney, and defense attorney to assess the
patient’s ability to work with counsel. At any point during the treatment program, the
patient may be evaluated to confirm they are competent to stand trial. After evaluation, if
there is concurrence that the patient is competent, a forensic report is sent to the court,
identifying that the patient is competent and ready to stand trial. Because the focus of
IST treatment programs is the rapid restoration of competency for the purposes of
criminal proceedings, individualized, comprehensive treatment of patients’ mental health
disorders is not provided by this treatment pathway.
National Data and California Data
The exponential increase in individuals found IST across the country has left State-run
mental health systems, including the California Department of State Hospitals (DSH),
challenged to meet the demands of year-over-year increases in the number of IST
referrals to their systems. A 2017 study conducted by the National Association of State
Mental Health Program Directors Research Institute (NRI)
2
found that from 1999 to
2014, the overall number of forensic patients in state hospitals increased by 74% while
the number of IST patients increased by 72% during that same period. The following
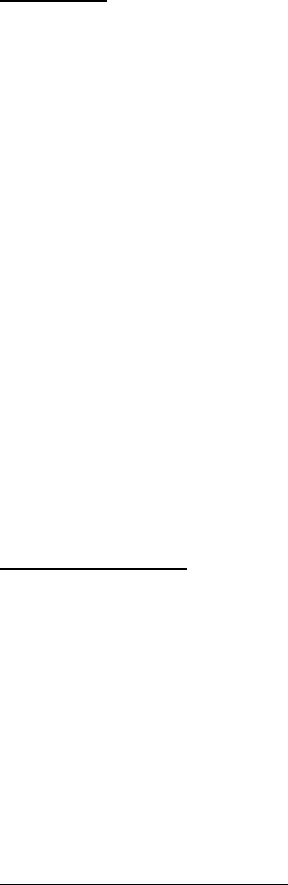
chart displays the percentage change overtime for 26 states:
2
Wik, A., Hollen, V., Fisher, W.H. (2017) Forensic Patients in State Psychiatric Hospitals: 1999-2016.
https://www.nasmhpd.org/sites/default/files/TACPaper.10.Forensic-Patients-in-State-Hospitals_508C_v2.pdf.
7
Multiple state hospital systems across the country are facing lawsuits because of their
inability to continuously increase the number of forensic inpatient beds available to
admit and treat IST patients within court mandated timeframes, including here in
California (Stiavetti v. Ahlin) which has set a 28-day post commitment deadline for DSH
to begin substantive treatment of an IST ordered to DSH. Most notably, in the State of
Washington (Trueblood v. Washington (2015)), the State has paid over $100,000,000 in
contempt fines because of its inability to meet court ordered timeframes for admission
into treatment programs largely because the demand for IST services has outpaced the
state’s efforts to develop capacity
3
. Under a recent change to the settlement
agreement, the fines are being redirected to support improved access to appropriate
behavioral health services that are designed to dramatically reduce the number
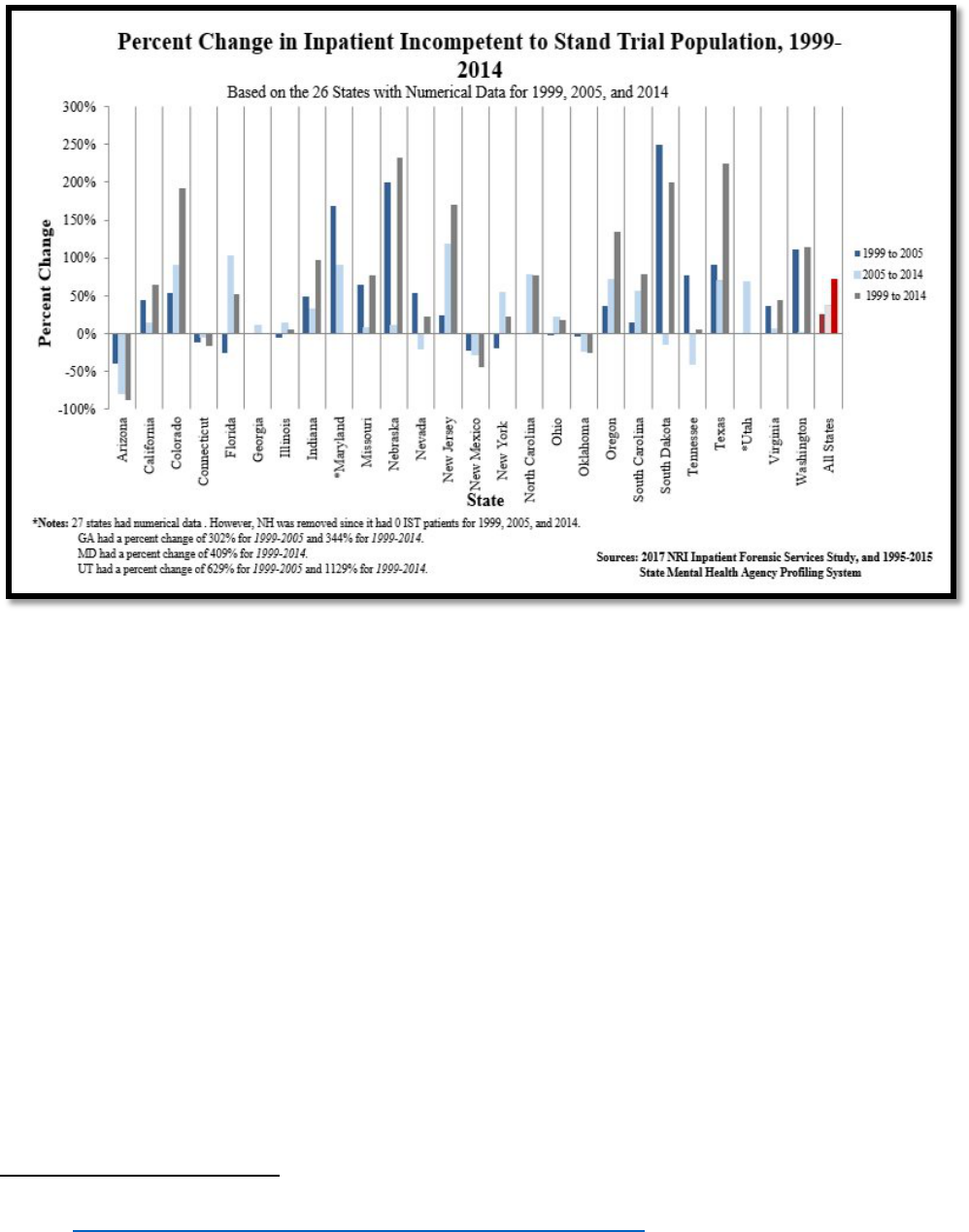
of people entering the criminal court system. However, as the following chart shows, as
Washington State has built out its forensic system in response to this suit, the referrals
3
From “Trueblood et al v. Washington State DSHS,” by Washington State Department of Social and Health
Services, https://www/dsjs/wa/gov/bha/trueblood-et-al-v-washington-state-dshs
. Retrieved November 22, 2021.
8
of IST patients have only continued to increase and, regardless of the funding made
available to the state system, capacity cannot keep up with demand
4
:
Unfortunately, the IST crisis in California has mirrored the crisis experienced across the
country. However, the size of California’s population has magnified the IST crisis in this
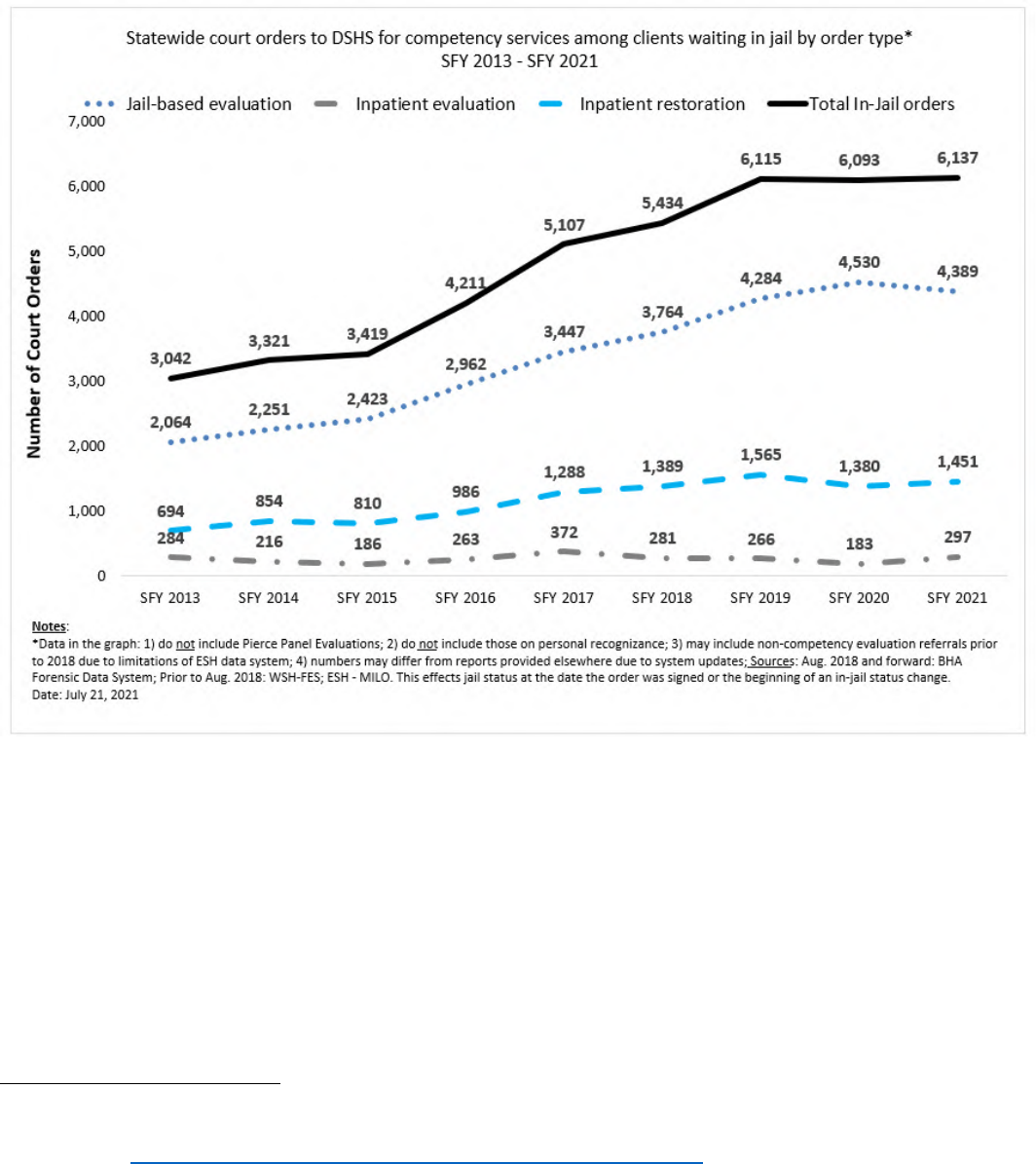
state. DSH first noted a substantial increase in IST referrals around 2013. Each year
since then, DSH has experienced growth in the number of IST referrals to the
department’s felony IST programs that has outpaced DSH’s efforts to increase capacity
to meet the demand for services resulting in a growing waitlist as displayed in the
following graph:
4
Chart displays growth in competency referral rates received by the Washington State Department of Social and
Health Services. From “Trueblood et al v. Washington State DSHS,” by Washington State Department of Social and
Health Services, https://www/dsjs/wa/gov/bha/trueblood-et-al-v-washington-state-dshs
. Retrieved November 22,
2021.
9
In 2020, while IST referrals decreased due to the global COVID-19 pandemic and
statewide Stay-in-Place orders, the IST treatment programs’ ability to admit new IST
patients were also significantly impacted by COVID-19 outbreaks and the necessary
infection control procedures implemented to protect patients and staff. In 2021-22, DSH
is again experiencing a high number of referrals from the courts that exceeds the pre-
pandemic referral rates, however, DSH must still maintain its implementation of COVID-
19 infection control practices as required by the California Department of Public Health.
These infection control measures as well as intermittent COVID-19 outbreaks continue
to limit the efficiency and the rate of admissions to its programs. As such, the waitlist
has grown to over 1700 individuals as of November 2021.
Individual Patient Characteristics
To better understand what was potentially driving the sustained increase in felony IST
referrals, DSH partnered with the University of California, Davis to study the IST
patients being admitted to Napa State Hospital. This review of DSH IST admissions
found the following:
• Between calendar years 2009 and 2016, the percent of IST patients admitted to
Napa State Hospital diagnosed with a psychotic disorder, psychosis NOS, or
mood disorder ranged from 72.5% to 84.1%. A small percentage of IST patients
were found to have a primary substance use disorder, cognitive disorder, or were
malingering.
• In 2009, 17.7% of IST patients admitted to Napa State Hospital had 16 or more
prior arrests. By 2016, the percentage of IST patients admitted to Napa State
Hospital with 16 or more prior arrests had increased to 46.4%.
• In 2016, approximately 47% of IST patients admitted to Napa State Hospital were
unsheltered homeless prior to their arrest. Between 2018 and 2020, 65.5% of
IST patients admitted to Napa State Hospital were homeless (sheltered or
unsheltered) prior to arrest.
10
• On average, 47% of IST patients admitted to Napa State Hospital had received
no Medi-Cal billable mental health services in the six months prior to arrest; 23%
had received one to two mental health services in emergency departments
(EDs); 20% had received three or more mental health ED services; and 10%
received no mental health ED services.
To provide some context to these findings, DSH and UC Davis conducted a national
survey asking state mental health officials about their states’ crisis. The responses
received were another indicator of the scale of the problem facing the nation: 68.8% of
survey respondents indicated the rate of referrals for competency restoration for
misdemeanor offenses was increasing in their state, 65.3% of respondents indicated
that the rate of referrals for competency restoration for felony offenses was increasing in
their state, and 78% of respondents indicated the rate of referrals for competency
restoration for felony and misdemeanor offenses were both increasing in their state. In
addition, 70.8% of respondents shared that their state hospital system has a waitlist for
admitting IST patients and 38.8% of respondents indicated that their state is currently
facing litigation related to the admission of IST patients into their system of care. Finally,
the survey asked respondents to rank what, in their experience, were the leading
causes of this crisis. Here are the top four responses ranked in order of impact to the
crisis:
• Inadequate general mental health services
• Inadequate crisis services in community
• Inadequate number of inpatient psychiatric beds in community
• Inadequate ACT services in community
The results of this national survey and the clinical review of the IST patients admitted to
DSH has led DSH to hypothesize that the drivers of this crisis are as follows:
• Individuals with Schizophrenia Spectrum Disorders are drifting into an untreated,
unsheltered condition.
• These conditions are leading to increased contact with police and
criminal charges.
• This increased contact is leading to a surge in IST referrals to state hospitals.
• Building more state hospital beds will only exacerbate the problem long term.
• IST restoration of competency treatment is not an adequate long-term treatment
plan.
Finally, DSH wanted to know if currently designed IST treatments impact or change the
trajectory of IST patients’ lives subsequent to discharge from DSH. DSH worked with
the California Department of Justice (DOJ) to obtain criminal offender record information

11
for IST patients discharged from DSH. The offender record information was then
matched with DSH discharge data and used to determine disposition outcomes for the
original IST commitment as well as to determine the rates of recidivism of individuals
post competency restoration at DSH. The analysis of DOJ and DSH data reflects how
the treatment provided by law to IST patients to restore competency does not have a
long-term positive impact for the individual and the community. Under existing law,
competency treatment is focused on the stabilization of an individual’s psychiatric
symptoms and basic legal education which together are intended to allow the defendant
to work with their attorney, understand the charges against them, and effectively
participate in their own defense.
DSH looked at the 3-year post discharge recidivism rates utilizing DOJ criminal offender
record information data and found a:
• 69% recidivism rate
5
for IST patients discharged from DSH in FY 2014-15
• 72.3% recidivism rate for IST patients discharged from DSH in FY 2015-16
• 71% recidivism rate for IST patients discharged from DSH in FY 2016-17
In examining the legal pathways of IST patients post competency restoration treatment
at DSH state hospitals and jail-based competency treatment programs, the data shows
that from FY 2016-17 through FY 2018-19 (6,048 IST discharges in total), 15% of felony
IST patients had a single offense and post discharge from DSH 35% had their charges
dropped (includes case dismissed, proceedings suspended, not guilty, acquitted). Over
the same period, 85% of felony IST patients had multiple offenses and post discharge
from DSH 24% had some or all their charges dropped. The full range of disposition
outcomes for the felony IST patients discharged over this period include the following:
27.8% were sentenced to jail/probation (served either concurrently or consecutively),
25.9% had their cases dismissed, 24.3% were sentenced to prison, 14.2% were
sentenced only to jail and 0.2% were found guilty of some or all of their charges but
found not guilty by reason of insanity (NGI) and committed to DSH for treatment rather
than prison.
In summary, what this analysis shows is that most individuals committed to DSH as an
IST are not sentenced to state prison or committed to DSH for longer-term treatment.
Most IST patients restored by DSH return to their county of commitment and serve time
in jail, are released on probation, or are simply released. The rate of arrests of
discharged IST patients shows that whatever circumstances led to an individual’s prior
arrest have likely not changed and most IST patients are stuck looping through the
criminal justice system and DSH.
5
Recidivism rate reflects percentage of individuals with new arrests after discharge from DSH. DSH focuses on
arrests instead of convictions because defendants are committed to DSH post-arrest but pre-conviction.
12
III. Department of State Hospitals’ Efforts to Date
Since FY 2012-13, DSH has made multiple efforts to mitigate the effects of increasing
IST referrals through capacity expansion, system improvements, and legislative
changes.
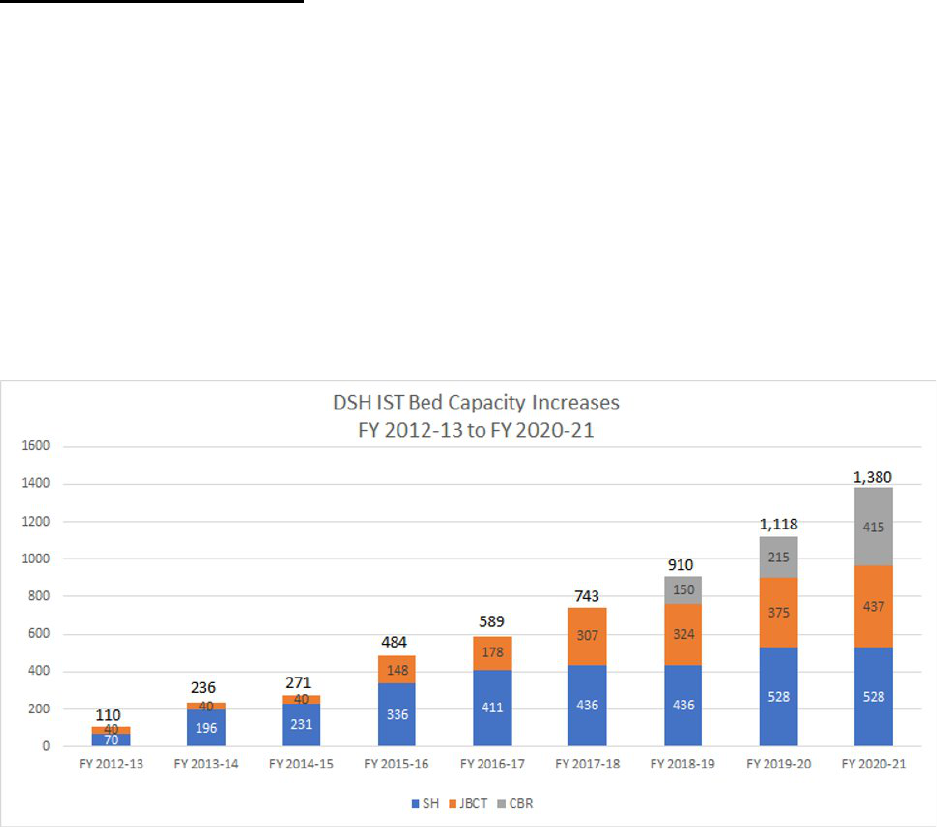
Increased Capacity at DSH
Since the beginning of the IST crisis, DSH has established new IST capacity through
the activation of 528 new state hospital beds, 445 jail-based treatment beds, 415
community-based restoration (CBR) beds, and a 78-bed Conditional Release Program
(CONREP) step down program (currently in progress). DSH is also in the process of
establishing 352 additional CBR beds and a CONREP Mobile Forensic Assertive
Community Treatment (FACT) Team to further expand DSH’s capacity to serve IST
patients. As the following table shows, in the first year of the crisis DSH added 110 beds
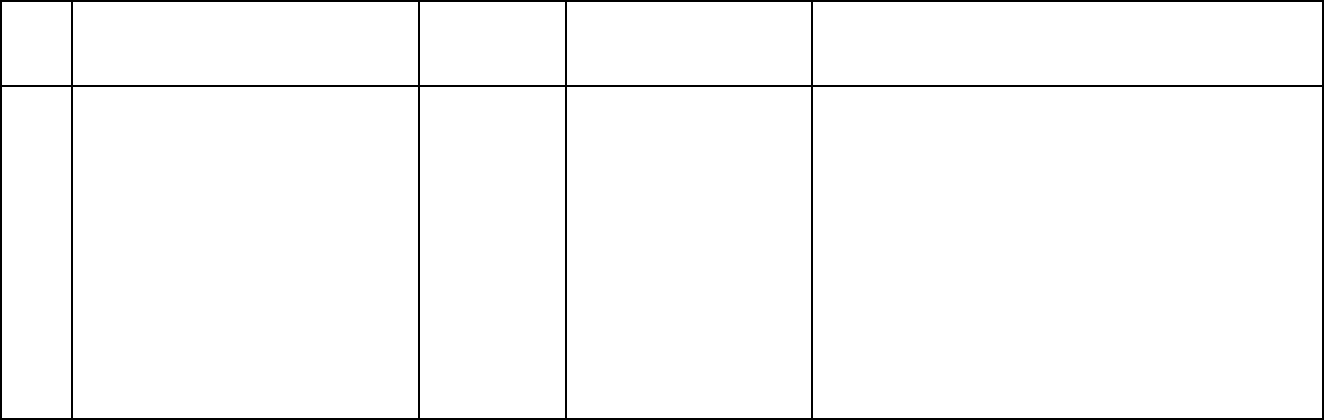
for IST treatment and by FY 2020-21 DSH had added a total of 1,380 beds between
State Hospitals (SH), Jail Based Competency Treatment (JBCT) programs, and the
Community Based Restoration (CBR) program:
In the 2021-22 budget, DSH was appropriated $255 million to create new sub-acute
capacity across the state to serve felony IST patients; $32.8 million to expand the CBR
program by 552 beds (300 in LA, of which 200 activated in spring 2021, and 252 across
the rest of the state); $47.6 million to expand the DSH Felony Mental Health Diversion
(Diversion) program (see pp. 17-18 for a detailed description of this program); $13.1
million to expand the department’s Jail Based Competency Treatment program
expansion and; $9.7 million to establish a Forensic Assertive Community Treatment
13
(FACT) program in CONREP to serve higher acuity patients, such as ISTs, in the
community.
In this budget, DSH also received $12.7 million to establish a four year, limited-term IST
Re-evaluation Program. This program establishes a temporary team of forensic
evaluators who will re-evaluate IST patients for competency who have been committed
to DSH and have been in jail for over 60 days. If an IST is evaluated and found to have
regained competency while in jail the IST Re-evaluation team will submit the
appropriate reports to the courts. Additionally, if the IST Re-evaluation identifies an IST
who has not restored to competency may be appropriate for the DSH Felony Mental
Health Diversion program or community-based restoration, the IST Re-evaluation team
can make a referral to these programs. The goal of this program is to address the
current waitlist of over 1,700 IST patients by bridging the gap between DSH’s current
capacity, the current rate of IST referrals, and the ongoing impacts of COVID-19 to
admissions and discharges to the State Hospitals while the department’s new
investments in community-based treatment are implemented.
As part of its efforts to increase the number of felony IST patients that receive treatment
each year, the Department contracts with 21 California counties to provide restoration of
competency services to IST patients in county jail facilities. Jail-Based Competency
Treatment (JBCT) programs are designed to treat IST patients with lower acuity and to
quickly restore them to trial competency, generally within 90 days. If a JBCT program is
unable to restore an IST patient to trial competency quickly, the patient can be referred
to a state hospital for longer-term IST treatment. DSH currently operates three JBCT
program models:
1. Dedicated bed model – serves IST patients from one specific county with an
established number of dedicated program beds.
2. Regional model - serves IST patients from multiple counties statewide with an
established number of dedicated program beds.
3. Small county model – serves 12 to 15 IST patients annually and does not have
dedicated program beds.
Funding for these programs includes patients’ rights advocacy services. The funding for
the patients’ rights advocacy services complies with Assembly Bill (AB) 103 (Statutes of
2017). AB 103 requires that all DSH patients have equal access to patients’ rights
advocacy resources, including IST patients who are admitted to JBCT programs.
Over the last few fiscal years, the Department has also focused efforts on expanding
the capacity of its CONREP program with the goal of stepping down more patients
committed to DSH as NGI or as Offenders with Mental Health Disorders (OMDs) to free
up additional beds within the State Hospitals for IST patients. CONREP is DSH’s
statewide system of community-based services for specified court-ordered forensic
individuals. Mandated as a State responsibility by the Governor's Mental Health
14
Initiative of 1984, the program began operations on January 1, 1986 and operates
pursuant to statutes in Welfare and Institutions Code (WIC) 4360 (a) and (b). The goal
of CONREP is to promote greater public protection in California’s communities via an
effective and standardized community outpatient treatment system. The CONREP Non-
Sexually Violent Predator (Non-SVP) population includes:
• Not Guilty by Reason of Insanity (NGI) (Penal Code (PC) 1026)
• Offender with a Mental Health Disorder (OMD) (both PC 2964 parolees who have
served a prison sentence and PC 2972 parolees who are civilly committed for at
least one year after their parole period ends). This category also includes the
Mentally Disordered Sex Offender (MDSO) commitment under WIC 6316
(repealed).
• Felony Incompetent to Stand Trial (IST) (PC 1370 patients who have been court-
approved for outpatient placement in lieu of state hospital placement)
Individuals suitable for CONREP may be recommended by the state hospital Medical
Director to the courts for outpatient treatment. Currently, DSH contracts with seven
county-operated and eight private organizations to provide outpatient treatment services
to non-Sexually Violent Predator clients in all 58 counties of the state.
DSH is partnering with several community-based providers to build out the continuum of
care and increase the availability of placement options dedicated to CONREP clients.
This expands the number of community beds available for patients who are ready for
outpatient treatment but still need a higher level of care within CONREP. These facilities
allow patients to step down into a lower restrictive environment and focus on the skills
necessary for independent living when transitioning to CONREP. The expansion of
CONREP capacity and patient placement allows DSH to backfill vacated state hospital
beds with pending IST placements who are not eligible for outpatient treatment.
Expanding the availability of beds to treat DSH patients is critical to providing timely
access to those requiring and awaiting treatment in higher acuity state hospital settings.
Current efforts in expanding residential placement options include:
• Authority to establish a dedicated 78-bed step-down program intended to address
higher-level needs and patient acuity and operated in a secured Institute for Mental
Disease (IMD) facility. The program was designed for state hospital patients ready
for CONREP in 18-24 months. This setting allows for OMD and NGI patients to
step down into a lower restrictive environment and provide the skills necessary for
a more independent living setting when transitioning to CONREP, thereby allowing
for the vacated state hospital beds to be backfilled by IST patients. This program
is pending official regulatory approval and necessary modifications to the facility
but is expected to be activated in late summer 2022.
• Recognizing the need for more step-down CONREP beds in northern California,
DSH received authority to partner with a new provider to establish a 10-bed IMD

15
program. Activation began in July 2020 and was expanded by an additional 10
beds in July 2021.
• Authorized in 2021 Budget Act, DSH received authority to partner with a provider
to establish a 180-bed Forensic Assertive Community Treatment (FACT) model of
care in CONREP that will provide 60 beds each in Northern California, Southern
California, and the Bay Area. This new level of care for CONREP will establish
residential beds where services will be delivered onsite allowing for placement of
individuals with higher needs. The program is designed to provide 24/7 services to
clients as needed to support client success and reduce the likelihood of
rehospitalization through de-escalation and crisis intervention practices.
Additionally, a FACT model of care can be used to place IST patients ordered to
CONREP where a community-based restoration program is not available. DSH
estimates program activation of the 60 Northern CA beds to occur in January 2022,
the 60 Southern CA beds to activate in early spring 2022, and the 60 Bay Area
beds to activate in early winter 2022.
• An augmentation of $1 million in the 2019 Budget Act to support general housing
costs being absorbed by CONREP providers.
Systems Improvements
The second strategy DSH has employed in its attempt to manage the escalating IST
crisis has been the implementation of multiple systems improvements that increase
DSH’s efficiency in admitting, treating, and discharging IST patients. Through these
efforts, the department has reduced the average length of stay (ALOS) for IST patients
to 148.7 days in a state hospital bed and 69.7 days in a jail-based competency bed. The
decrease in the ALOS for IST patients is the result of improved utilization management
at the state hospitals (a process by which treatment is matched to a patient’s specific
clinical needs), the creation of the Patient Management Unit, and multiple legislative
changes that supported each of these efforts.
The Patient Management Unit (PMU) was established in June 2017 in the Welfare and
Institutions Code 7234 through Assembly Bill 103 (Chapter 17, Statutes of 2017) to
provide centralized management, oversight, and coordination of the referral and patient
pre-admission processes to ensure placement of patients in the most appropriate
setting based on clinical and safety needs. Prior to the establishment of the PMU, the
court system was able to order commitments to any DSH hospital of its choosing,
creating admission backlogs and inefficiencies. Now, PMU receives all court
commitments to the department and utilizes DSH’s Patient Reservation Tracking
System (PaRTS) to manage the admissions of all DSH patients.
Finally, multiple legislative changes have been made to support the department’s efforts
to maximize the use of each DSH-funded bed:
• AB 2186 (Chapter 733, Statutes of 2014) – Involuntary Medication Orders and
Court Reports
16
o Amended the law to require courts to reassess the authorization of
Involuntary Medication Orders (IMOs) upon the filing of the initial
competency progress report and any ongoing progress reports to the court
and that a petition may be filed within 60 days of the expiration of the one-
year IMO. This change created efficiency and consistency in the
application for and use of IMOs at DSH. The use of medications is a core
component of the treatment of IST patients
• AB 2625 (Statutes of 2014) – Unlikely to Regain Competency and Unrestored
Defendants – 10 Days to Return to Court
o Amended the law to require that IST patients who are determined to be
unlikely to restore to competency be returned to court within 10 days and
required that IST patients who had been committed to DSH up to the
maximum time allowed by law (in 2014, the maximum length of
commitment to DSH for an IST defendant was 3 years) to be returned to
court 90 days prior to the expiration of their commitment. This change
was intended to help DSH discharge patients more quickly so additional
IST patients could be admitted into the system, increasing the number of
IST patients that could be treated per year.
• AB 1810 (Statutes of 2018) – Prevents Transfer of Competent Defendants to
DSH
o Amended the law to allow courts to order a re-evaluation of an
IST defendant pending transfer to a State Hospital if they receive
information from the jail treatment provider or defendant’s counsel that the
defendant may no longer be incompetent. DSH found that a significant
number of IST patients committed to DSH had regained competency prior
to admission to DSH; this change was intended to prevent the transport
and admission of IST patients who had regained competency and
maintain limited DSH resources for those who were still IST.
• SB 1187 (Statutes of 2018) - Reduced the maximum length of stay for felony IST
patients from 3 years to 2 years.
o Amended the law to reduce the maximum commitment of IST patients to
DSH from 3 years to 2 years. This change was intended to discharge
patients from limited DSH beds more expeditiously to admit additional IST
patients and increase the potential number of IST patients served in a
year.
• Assembly Bill 133 (Statutes of 2021) – Misdemeanor IST Patients and Charges
for Non-Restorable IST Patients
o Amended the law to remove DSH as a county placement option for IST
patients with misdemeanor charges to preserve all appropriate state
17
hospital beds for felony IST patients. Also amended law to charge
counties a daily bed rate for IST patients that have been found non-
restorable that are not transported from DSH by the county within the
statutorily required 10-day timeframe.
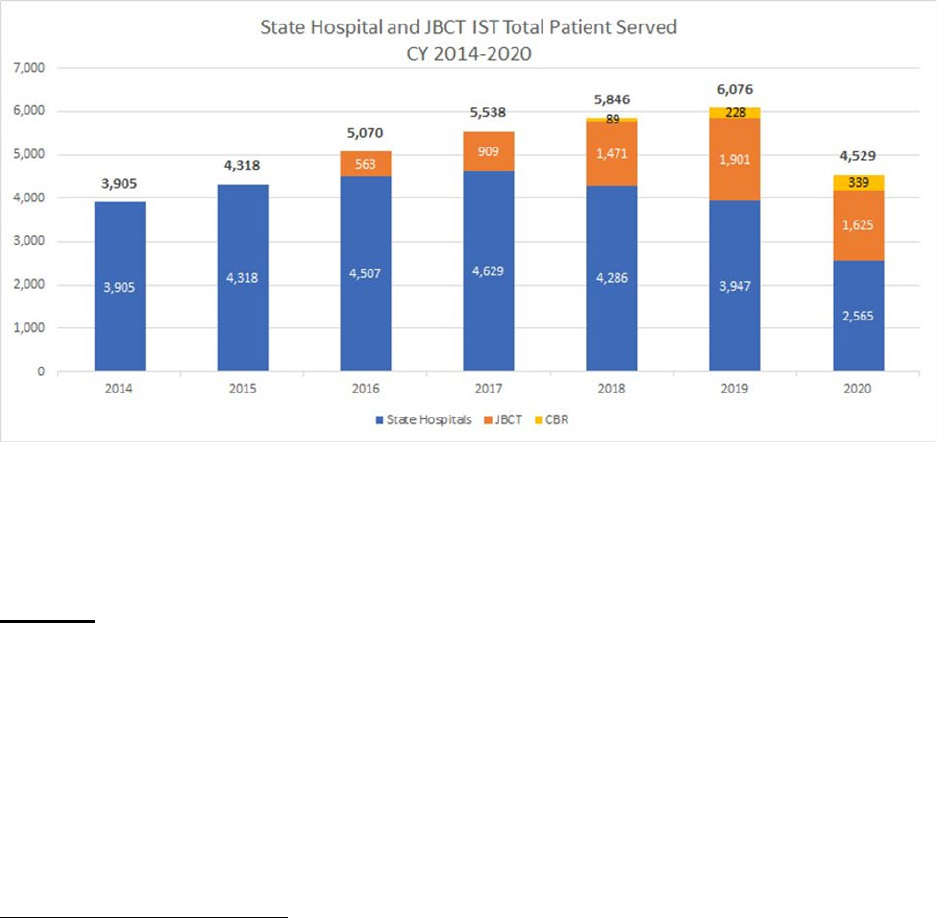
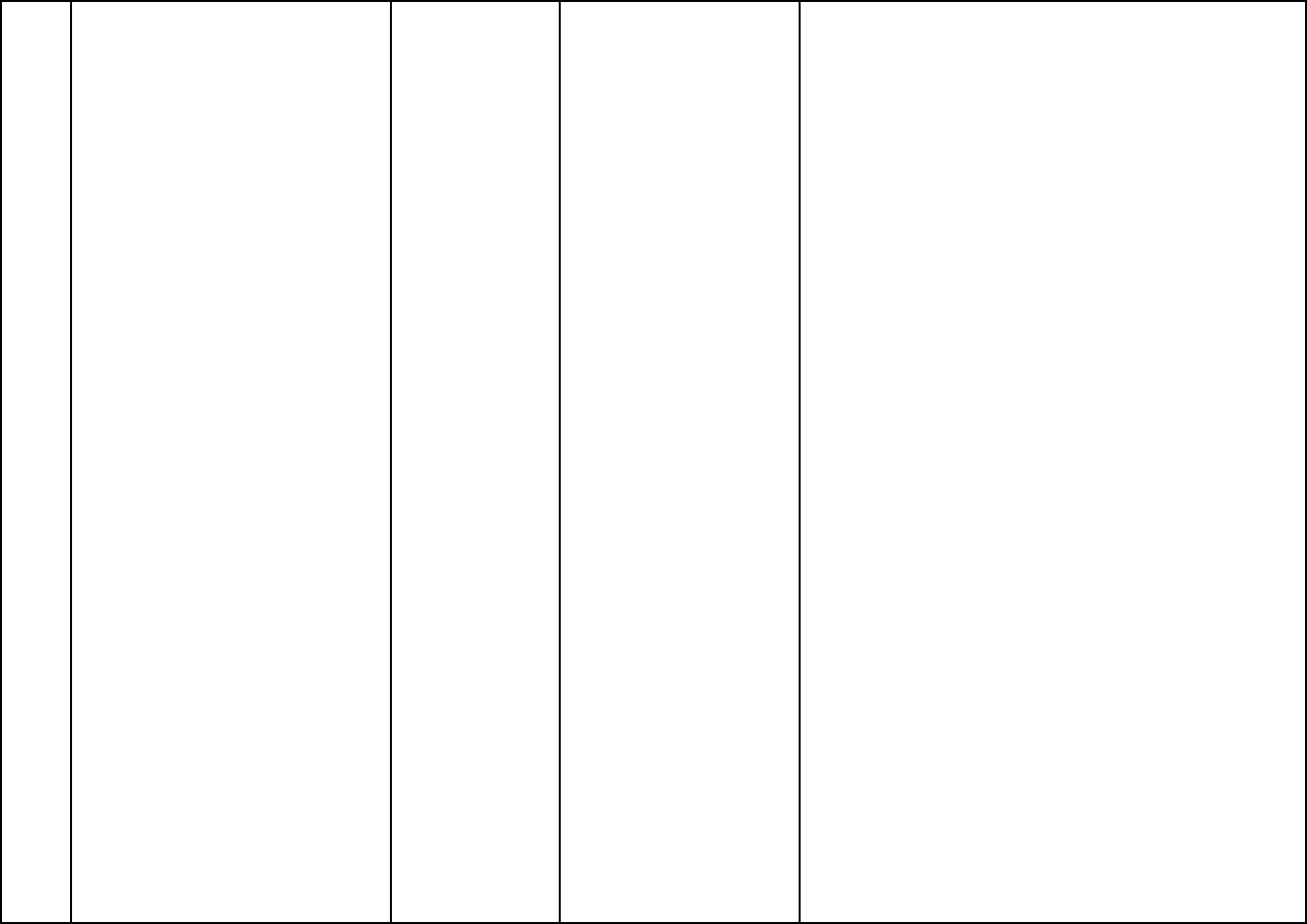
Each of these systems improvements has helped DSH reduce the length of stay of IST
patients in a DSH bed and, in conjunction with the capacity DSH has added to its
system of care, allowed the department to increase the number of IST commitments
served year-over-year
6
:
However, the demand for IST treatment has continued to outpace all efforts to create
enough capacity and system efficiency to reduce the number of IST patients pending
placement to DSH and reduce the length of time between commitment to the
department and receipt of substantive competency treatment.
Demand
By FY 2017-18, DSH recognized that the demand for IST treatment services was not
going to be met by capacity created within the State Hospital system. At this time the
department began working to establish treatment pathways in the community with the
long-term goal of decreasing demand for State Hospital services by connecting more
people with Serious Mental Illness into ongoing community care. The Budget Act of
2018 included funding for two major new programs to help DSH realize this vision.
The Budget Act of 2018 allocated $13.1million for DSH to contract with the Los Angeles
County Office of Diversion and Reentry (ODR) for the first community-based restoration
6
The table below, “State Hospital and JBCT IST Total Patients Served” reflects a drop in total patients served in
2020; this anomaly was caused by the SARS COVID-19 pandemic. State Hospitals ability to admit and discharge
patients during the first twelve months of the pandemic was significantly limited by necessary infection-control
measures taken by the Department to protect patients and staff in its congregate living treatment environment.

18
(CBR) program in the state. In this program, ODR subcontracts for housing and
treatment services for IST patients in the community. Most IST patients in this program
live in unlocked residential settings with wraparound treatment services provided on
site. The original CBR program provided funding for 150 beds; investments in the LA
program since 2018 has increased the program size to 515 beds. In addition, DSH has
received funding to implement additional CBR programs across the state. The Budget
Act of 2021 included ongoing funding to add an additional 252 CBR beds in counties
outside of Los Angeles, bringing the total number of funded CBR beds to 767.
The Budget Act of 2018 also allocated DSH $100 million (one-time) to establish the
DSH Felony Mental Health Diversion (Diversion) pilot program. Of this funding, $99.5
million was earmarked to send directly to counties that chose to contract with DSH to
establish a pilot Diversion program (the remaining $500,000 was for program
administration and data collection support at DSH). Assembly Bill 1810 (2018)
established the legal (Penal Code (PC) 1001.35-1001.36) and programmatic (Welfare &
Institutions Code (WIC) 4361) infrastructure to authorize general mental health diversion
and the DSH-funded Diversion program. The original Diversion pilot program includes
24 counties who have committed to serving up to 820 individuals over the course of
their three-year pilot programs. In FY 2021-22, DSH received additional funding to
expand this pilot program as follows:
• $17.4 million to expand current county contracts by up to 20%; WIC 4361
updated to require any expansion be dedicated to diverting defendants who
have been found IST by the courts and committed to DSH
• $29.0 million to implement diversion programs in any other county interested in
contracting with DSH
The goal of both the CBR and Diversion programs is to demonstrate that many of the
individuals committed to DSH as IST patients can be treated effectively and safely in the
community. Since launching these programs in 2018, DSH has partnered with some of
the most preeminent authorities in the treatment of individuals with Serious Mental
Illnesses and criminal justice involvement to provide technical assistance and training
for counties across the state implementing a DSH Diversion program and has shared
many of those resources with all counties, regardless of their participation in the DSH
program, through the Diversion program’s public webpage:
https://www.dsh.ca.gov/Treatment/DSH_Diversion_Program.html
Since 2018, DSH has provide over 100 hours of free training and technical assistance
to counties and continues to build out the resources it has to offer as the CBR and
Diversion programs grow. As of June 30, 2021, counties participating in the Diversion
pilot had diverted 458 individuals (some had been found IST and some were defendants
the county determined to be likely-to-be IST) and the Los Angeles CBR program had
served 641 IST patients.
19
IV. IST Solutions Workgroup Process
In accordance with Assembly Bill 133 and the 2021 Budget Act, the California Health
and Human Services Agency (CalHHS) and DSH established a statewide IST Solutions
Workgroup in August 2021. The IST Solutions Workgroup members were appointed by
CalHHS Secretary Mark Ghaly and the composition of the Workgroup, as required in
statute, included representatives from several state agencies, the Judicial Council, local
government and criminal justice system representatives, and representatives of IST
patients and their family members.
This Workgroup met five times (8/17/2021, 8/31/2021, 10/12/2021, 11/5/2021,
11/19/2021) as part of the IST solutions development process. To advance the
development of short-, medium-, and long-term strategies, three sub-working groups
were established that focused on specific areas of opportunity (See Appendix A for a full
list of working group members). All three groups were called on to focus all
recommendations of short-term solutions on the individuals currently on the waitlist.
These three working groups generated strategies for consideration by the full IST
Solutions Workgroup for inclusion in the final report to CalHHS and DOF. The three
topic-focused working groups included:
Working Group 1: Early Access to Treatment and Stabilization for Individuals
Found Felony IST
The goal of Working Group 1 was to identify short-term solutions to provide early
access to treatment and stabilization in jail or via Jail Based Competency Treatment
(JBCT) programs to maximize re-evaluation, diversion or other community-based
treatment opportunities and reduce IST length-of-stay in jails. Working Group 1 met on
9/21/2021, 9/28/2021, and 10/26/2021.
Working Group 2: Diversion and Community-Based Restoration for Felony ISTs
The goal of Working Group 2 was to identify short, medium, and long-term strategies to
maximize the implementation of IST Diversion and Community-Based Restoration
(CBR) programs across the state. Working Group 2 met on 9/24/2021, 10/1/2021, and
10/22/2021.
Working Group 3: Initial County Competency Evaluations
The goal of Working Group 3 was to identify solutions to reduce the overall number of
individuals found IST by strengthening the quality of the initial competency evaluations
ordered by the courts (also known as alienist evaluations). Working Group 3 met on
9/17/2021, 9/24/2021, and 10/15/2021.
Due to COVID restrictions and the tight time frame of the process, meetings were held
virtually using Zoom technology that enabled full participation of all members, as well as
the public, who were routinely invited to comment using the Zoom “chat” feature, as well

20
as verbally as time permitted. The goal was to establish a transparent and inclusive
process that allowed active participation from a diverse spectrum of participants. All
meetings followed the requirements of the Bagley-Keene Open Meeting Act.
Meeting agendas, presentations, written input from members and the public, responses
to information requests, and meeting minutes from the IST Solutions Workgroup and the
three topic-focused working groups are available on the IST Solutions Workgroup web
site.
Guiding Principles for Generating Recommendations
The statute provided guidance for what the IST Workgroup solutions should focus on
when generating solutions to the IST crisis. This guidance included:
1. Reduce the total number of felony defendants determined to be IST
2. Reduce the lengths of stay for felony IST patients
3. Support felony IST defendants to receive early access to treatment before
transfer to a restoration of competency treatment program to achieve stabilization
and restoration of competency sooner.
4. Support increased access to felony IST diversion options.
5. Expand treatment options for felony IST individuals, such as community-based
restoration programs, jail-based competency treatment programs, and state
hospital beds.
6. Create new options for treatment of felony IST defendants including community-
based, locked, and unlocked facilities.
7. Establish partnerships to facilitate admissions and discharges to reduce
recidivism and ensure that the most acute, high-risk, and at need patients receive
access to State Department of State Hospitals beds, while patients with lower
risk of acuity are treated in appropriate community settings.
In addition to this statutory guidance, the IST Solutions Workgroup adopted the
following guiding principles to frame its recommendations:
• Mental health treatment should be delivered in community-based treatment
options to the greatest extent possible.
• While jail is not the appropriate setting for mental health treatment, jails need to
be able to provide mental health treatment for individuals who are in jail and
require treatment.
• Engagement of individuals with lived experience and family members in planning
and implementing solutions and programs is critical.

21
• Short-term solutions focus on treating the 1700+ individuals found incompetent to
stand trial on felony charges and waiting in jail for access to treatment or
diversion programs.
• Medium-term solutions focus on increasing access to community-based
treatment and diversion for individuals found incompetent to stand trial on felony
charges.
• Long-term solutions aim for system transformation and to reverse the trend of
criminalizing mental illness.
• Implementing solutions to achieve the short-, medium- and long-term goals
requires collective, multi-sector solutions and collaboration.
• To address the current IST crisis, implementation of short-term strategies that
are not in alignment with long-term goals may be needed, but should be time-
limited, phased out when medium- and long-term solutions are implemented, and
not detract from the focus and implementation of the long-term goals.
Process for Synthesizing Recommended Solutions
Over the course of the topic-focused working group meetings, more than 100 potential
solutions were generated by members and the public through an iterative process of
idea generation, reflection, and refinement within each of the three working groups, as
well as the larger Workgroup. Additionally, these solutions were assessed to determine
which were most feasible, actionable, and relevant to addressing the short-, medium-,
and long-term timeframes and goals, which enabled the team to reduce and consolidate
the total number of potential solutions from 100 to ~35. Any recommendation that did
not represent an actionable solution was not included. A draft compilation of the
solutions was presented to the full workgroup for discussion. Through that discussion
and additional solutions submitted from workgroup members and other organizations
and members of the public who participated in the meetings, a final list of 41
recommended solutions was generated to be presented to the CalHSS and DOF.
22
V. Census of Recommended Solutions from the IST Workgroup Meetings for Submission to CalHHS and
Department of Finance
Short Term Strategies: Solutions that can begin implementation by April 1, 2022
Goals:
a. Provide immediate solutions for 1700+ individuals currently found incompetent to stand trial on felony charges and
waiting in jail for access to a treatment program.
b. Provide quick access to treatment in jail, the community, or a diversion program.
c. Identify those who have already restored.
d. Reduce new IST referrals.
#
Strategy
Type
Potential Impact
Other Considerations
S.1
Support increased access to
psychiatric care, including
stabilizing medications in jail
for felony ISTs while pending
transfer to other IST treatment
programs or when returning
from IST treatment programs
to jail pending court
proceedings, including:
• Provide funding to jails
to expand the use of
long-acting injectable
psychiatric medications
(LAIs) in jail settings.
• Use of
technology/telehealth
for jail clinicians to
access tele-
Funding/
Policy
Provides
opportunities for
faster stabilization of
mental health
symptoms in jail and
increase
opportunities for
individuals to be
candidates for
Diversion or
community-based
restoration
programs. While jails
are not the
recommended
treatment setting,
recognizes there is
an immediate crisis
Jails do not receive state funding support for
treatment and housing of individuals found
IST on felony charges unless they have been
admitted to a DSH-funded jail-based
competency treatment program. However,
individuals who have been deemed
incompetent to stand trial on felony charges
and are not yet transferred to a Diversion or
other treatment program should receive
appropriate mental health treatment until they
are transferred to a treatment program.
Funding to jails to support the resources and
costs to providing these services may also
need to be considered.
Jail formularies may need to be updated to
include long-acting injectable medications
(LAIs).
23
psychiatrists to provide
medication/treatment
determinations,
including involuntary
medications, when
necessary, ordered by
the court and
appropriate due
process procedures are
followed.
• Increase opportunities
to rapidly connect a
court-appointed
competency evaluator’s
opinion that a patient
needs medication to jail
providers for
consideration in an
individual’s treatment
plan.
• Support training
opportunities for jail
clinicians on patient
engagement, including
rapport building skills
and motivational
interviewing.
and responses must
address the crisis in
the short-term.
There is not
currently sufficient
community capacity
for stabilization of
acute mental health
conditions.
Individuals who are
currently waiting in
jail for admittance to
treatment programs
are more likely to
access treatment in
existing Diversion
and community-
based restoration
programs if their
acute mental health
symptoms are
rapidly stabilized.
Lack of symptom
stabilization has
been identified as
the primary barrier to
Department of State
Hospitals (DSH) IST
Diversion Program
placement.
S.2
Improve coordination between
State, criminal justice
Operations/
Funding
Increased
partnership and
Short-term bridge solutions may need to be
implemented to advance these solutions until
24
partners, county
behavioral/mental health
directors, and county public
guardians, for IST patients,
including:
• Transition/treatment
planning to ensure
continuity of care
between systems and
providers.
• Providing a 90-day
medication supply for
individuals discharging
to the community from
jail, Diversion, or
restoration of
competency treatment
programs.
• Use of common drug
formularies, wherever
possible.
• Data sharing/use of
business associate
agreements.
• Identifying community
based and Diversion
alternatives.
opportunities for
Diversion and
community-based
treatment for felony
ISTs. Increased
support for
transitions and re-
entry after felony IST
finding or release to
reduce
destabilization and
re-arrest.
the CalAIM reforms, addressing enrollment in
Medi-Cal prior to release and enhanced care
management, noted in Strategy L.2 are
implemented.
Individuals with mental illness, family
members, and advocates should be included
in stakeholder discussions about how best to
coordinate these efforts.
S.3
Provide training and technical
assistance and develop best
practice guides (toolkits) for
jail clinical staff, criminal
justice partners, boards of
supervisors, and county
Training
Increased early
treatment
engagement and
stabilization of
individuals will
reduce the
DSH Clinical Operations is actively providing
technical assistance and training, as well as
psychopharmacology consultation, to any
county partners who request it.

25
administrators for
understanding and
implementing effective
treatment engagement
strategies including:
• Seeking treatment and
medication histories
from family members.
• Utilization of incentives
and other strategies to
engage treatment
including best practices
for developing
patient/clinician
rapport, continuity, and
securing the voluntary
consent to medication
whenever possible.
• Obtaining involuntary
medication orders and
administering
involuntary
medications, when
necessary, ordered by
the court, and
appropriate due
process procedures are
followed.
symptoms of
psychosis such as
hallucinations,
delusions, and
disorganized
thinking. This will
provide increased
opportunity for
placement in
Diversion or
community-based
restoration
programs, as well as
decrease the length
of stay for individuals
on the pathway to
JBCT or State
Hospital placement.
This recommendation focuses primarily on
training and technical assistance needs.
Implementation of these strategies may
require funding or other support.
S.4
Re-assess the DSH current
waitlist, in partnership with
DSH, county behavioral
health, jail treatment
providers, and criminal justice
Operations
Reduce current
waitlist and increase
access to
community-based
The 2021 Budget Act included funding for
DSH to re-evaluate individuals on the IST
waitlist after 60 days to determine if an
individual has been restored to competency
or stabilized enough to be considered for
26
partners to identify individuals
who may be eligible for
release into community
treatment programs such as
MH Diversion, DSH IST
Diversion, CONREP or
community-based restoration,
address medication/treatment
needs to stabilize mental
health symptoms in jail,
identifying individuals who,
due to their psychiatric acuity,
may need priority transfer to a
state hospital pursuant to
California Code of
Regulations Section 4177,
and swiftly move individuals
into these programs to
maximize their utilization.
treatment for felony
ISTs.
Diversion or CONREP placement. Further
opportunities exist to actively partner with
counties prior to 60 days to identify
individuals who may be candidates for
placements in Diversion/CONREP.
S.5
Expand technical assistance
for Diversion and community-
based Restoration, including:
• Developing best
practice guides in
partnership with key
stakeholders.
• Providing training and
technical assistance to
newly developing
programs.
• Providing training and
technical assistance on
Training
Supports increased
utilization and
expansion of
Diversion and
community-based
treatment options for
felony ISTs.
DSH developed and implemented a Diversion
Academy for counties who plan to implement
DSH Diversion programs for ISTs. This was
offered in the fall 2021 to counties who have
applied for funding to establish new Diversion
programs. DSH also maintains a website of
technical assistance resources to support
Diversion. Additionally, DSH plans to expand
technical assistance opportunities to counties
to support implementation of community-
based restoration programs.
27
options to assess and
mitigate public safety
risks.
S.6
Provide training and technical
assistance for Court
appointed evaluators to
improve the quality of the
reports used by courts in
determining a defendant is
incompetent to stand trial:
• Develop checklists for
court appointed
evaluators to follow of
items to be considered
when making
competency
recommendations,
including American
Academy of Psychiatry
and the Law guidelines
and/or Judicial Council
rules of Court and
considering defense
counsel observations
and concerns regarding
their client’s ability to
participate rationally in
their defense.
• Develop template
evaluation reports that
include all checklist
items, including short-
form report options for
Training
Improves quality of
court-appointed
evaluator reports to
inform the court
whether an
individual may be
incompetent to stand
trial and the basis of
that determination
including an
individual’s
diagnosis, whether
they require an
involuntary
medication order
(IMO), or if they are
malingering
symptoms. May
reduce the number
of individuals found
incompetent to stand
trial and increase
access to treatment
and stabilization
when treatment
engagement is
difficult due to an
individual’s severe
symptoms of
psychosis.
This recommendation focuses primarily on
training and technical assistance needs.
Implementation of these strategies may
require funding or other support.

28
when clinically
appropriate
• Develop technical
assistance and training
videos to increase
knowledge and skills
for existing court
appointed evaluators,
including principles of
community based
mental healthcare,
which can be available
on DSH website.
• Ensure training and
technical assistance
includes information on
discrepancies and
biases in evaluations.
S.7
Prioritize community-based
restoration and Diversion by:
• Allowing individuals
placed into Diversion to
retain their place on the
waitlist should they be
unsuccessful in
Diversion and need
inpatient restoration of
competency services.
• Improving
communication
between DSH and local
courts in collaboration
Policy
Addresses concerns
from Diversion
providers that
individuals will not
have timely access
to a DSH treatment
program if the
individual’s mental
health symptoms
and community
safety risk
significantly
increases.
Additionally, reduces
DSH issued Departmental Letter 21-001 on
November 3, 2021, to implement this
recommendation. It outlines the process to
facilitate coordination between Diversion
programs, the courts, and DSH when an
individual is being considered for Diversion to
ensure the individual is not inadvertently
transferred to a DSH hospital or jail-based
competency treatment program. It also
establishes the procedure for a Diversion
program client to reenter the waitlist with their
original commitment date when an individual
is revoked from Diversion and needs to be
transferred into a secure treatment program.
29
with the Judicial
Council so that a
person on the waitlist is
not removed from
Diversion consideration
prematurely when a
bed becomes available
at DSH.
instances where
individuals are
transferred to a DSH
hospital or JBCT
pre-maturely when
an individual is being
considered for
Diversion.
S.8
Prioritize and/or incentivize
DSH Diversion funding to
support diverting eligible
individuals from the DSH
waitlist.
Policy/
Statutory
Assists in reducing
the DSH waitlist by
prioritizing
individuals on the
waitlist for Diversion
over individuals
likely to be found
incompetent to stand
trial. Individuals
likely to be found
incompetent to stand
trial are also eligible
for DSH Diversion.
The 2021 Budget Act included funding for
existing programs to expand Diversion
programs to divert individuals who have been
found incompetent to stand trial on felony
charges from DSH waitlist. Welfare and
Institutions Code 4136 by trailer bill, SB 129
(Committee on Budget, Statutes of 2021),
also amended to prioritize expansion funding
to individuals found incompetent to stand trial.
S.9
Include justice-involved
individuals with serious mental
illness as priorities in state-
level homelessness housing,
behavioral health, and
community care infrastructure
expansion funding
opportunities
Policy
Supports increased
access to
community-based
treatment for justice-
involved individuals
including felony
ISTs.
While funding and capacity expansion are
longer-term strategies, inclusion in priorities
and planning that is underway now or in the
short-term should occur.
S.10
Augment funding in DSH
Diversion contracts with
counties to provide for interim
housing, including subsidies,
Funding
Addresses concerns
of DSH Diversion
program providers
about insufficient
30
and housing-related costs to
support increased placements
into Diversion.
funding to access
housing for the DSH
Diversion population
S.11
Local planning efforts for
homelessness housing,
behavioral health continuum,
and community care
expansion should include
behavioral health and
criminal-justice partners and
consider providing services for
justice-involved individuals
with Serious Mental Illness to
reduce homelessness and the
cycle of criminalization.
Policy
Supports local
efforts and inclusion
of justice-involved
individuals in
planning and
strategy
development for
local investments
and state-level
grants.
31
Medium-Term Strategies: Solutions that can begin implementation by January 10, 2023
Goals:
a. Continue to provide timely access to treatment.
b. Begin to implement other changes that address broader goals of reducing the number of ISTs.
c. Increase IST treatment alternatives.
#
Strategy
Type
Potential Impact
Other Considerations
32
Statutorily prioritize
community outpatient
treatment and Diversion for
individuals found
incompetent to stand trial on
felony charges for
individuals with less severe
behavioral health needs and
criminogenic risk, and
reserve jail-based
competency and state
hospital treatment for
individuals with the highest
needs. Options include:
• Require
consideration of
Diversion for anyone
found incompetent to
stand trial on felony
charges.
• Treat penal code
1170(h) felonies, for
which the maximum
penalty is a prison
term served in the
county jail rather than
in state prison,
consistent with SB
317 (Chapter 599,
Statutes of 2021)
which requires a
hearing for Diversion
eligibility, if not
Statutory/
Funding
Establishes priority
for Diversion and
community-based
treatment for felony
ISTs whenever
appropriate based
on an individual’s
treatment needs and
criminogenic risk.
Prioritizes utilization
of state-hospital and
jail-based
competency
treatment programs
for those with the
highest needs.
Corresponding operational changes could be
implemented to also develop clinical factors
for determination of treatment in State
hospitals versus jail-based competency
treatment programs. Currently, over referral
to state hospitals and jail-based competency
treatment programs and under-utilization of
Diversion programs and lack of community-
based treatment programs results in lengthy
waitlists and inefficient utilization of inpatient
and jail-based beds.
Implementation of statutory changes may
require funding or other supports related to
court hearings and treatment capacity.
33
Diversion eligible, a
hearing to consider
assisted outpatient
treatment,
conservatorship, or
dismissal of the
charges.
• Change presumption
of appropriate
placement to
outpatient treatment
or Diversion for
felony IST, require
judicial determination
based on clinical
needs or high
community safety
risk for placement at
DSH or in a jail-
based treatment
program, and a
determination that
community resources
are available to meet
the treatment needs
of the individual.
• Reform exclusion
criteria of Diversion
under PC 1001.36 to
“clear and present
risk to public safety”
rather than
criteria of Diversion under PC 1001.36 to
“clear and present risk to public safety”
rather than "unreasonable risk to public
safety."
34
“unreasonable risk to
public safety.”
• Statutorily require the
use of structured
mental health risk
assessments to
assist in identifying
defendants that
should be eligible for
Diversion or
community
treatment.
• Require judicial
consideration of
Diversion at the
outset of criminal
proceedings for
mentally ill
defendants.
• Eliminate the
requirement of a
nexus between the
defendant’s mental
disorder and the
charged offense for
individuals diagnosed
with a serious mental
illness or establishing
a rebuttable
presumption of
nexus.
• Establish a
presumption of
35
Diversion eligibility if
an individual is
determined to be
incompetent to stand
trial and meets
clinical and legal
eligibility, subject to
the availability of a
treatment plan.
Establish a presumption of Diversion
eligibility if an individual
is determined to be
incompetent to stand trial
and meets clinical and legal
eligibility, subject to the
availability of a treatment
plan.
36
M.2
Provide increased
opportunities and dedicated
funding for intensive
community treatment
models for individuals found
IST on felony charges.
Options include:
• Assisted Outpatient
Treatment (AOT)
• Forensic Assertive
Community
Treatment (FACT)
• Full-Service
Partnerships (FSP)
• Regional community-
based treatment and
Diversion programs
for individuals not
tied to any one
county
• Crisis Residential
• Substance abuse
residential treatment
• Psychiatric health
facilities
• Mental Health
Rehabilitation
Centers
• Transitional
residential treatment
Funding/
Policy
Increases access to
community-based
treatment
alternatives for
justice-involved
individuals with
serious mental
illnesses and
reduces the
incarceration.
M.3
Establish a new category of
forensic Assisted Outpatient
Statutory
Increases access to
community-based
treatment
Establishing category would be a medium-
term strategy. However, implementing
programs would be a long-term strategy.
37
Treatment commitment that
includes:
• Housing
• Long-acting
injectable psychiatric
medication
• Involuntary
medication orders,
when necessary, as
ordered by the court,
and appropriate due
process procedures
are followed.
• FACT team
• Intensive case
management
alternatives for
justice-involved
individuals with
serious mental
illnesses and
reduces the
incarceration. A
forensic AOT
commitment would
ensure access to,
and engagement
with an intensive
level of outpatient
services designed to
interrupt the cycle of
criminalization in
lieu of inpatient
restoration
commitment.
M.4
Establishing statewide pool
of court-appointed
evaluators and increase the
number of qualified
evaluators:
• Request counties to
share their lists of
court-appointed
evaluators.
• Identify
demographics and
cultural and linguistic
competence of
evaluators.
Funding/
Operations
Assists courts in
access to expanded
statewide pool of
court-appointed
evaluators and
potentially reduces
the amount of time
individuals wait in
jail for a court-
appointed
evaluation.
Establishing a
diverse pool of court
appointed
38
• Increase court
funding for court
appointed evaluator
pay.
evaluators reduces
the risk that
individuals are
determined to be
incompetent to
stand trial due to
cultural and
linguistic
differences.
M.5
Improve statutory process
leading to finding of
incompetence or restoration
to competence:
• Set time frames for
appointments of
court appointed
evaluators and
receipt of reports.
• Set statewide
standards for court
evaluations and
reports.
• Expand list of
individuals who can
recommend to the
court a need for re-
evaluation if
someone may have
been restored –
noted already
authorized for those
over 60 days.
Statutory
Reduces time in jail
for individuals
awaiting
competency
assessments and
increases quality of
court-appointed
evaluator reports.
Allows an individual
to be reevaluated for
competency after
the initial finding and
before transfer to a
treatment program.
Penal Code 1370 in 2019 was amended to
allow jail providers and public defenders to
request the court to appoint an evaluator to
reevaluate a person’s competency. Welfare
and Institutions Code 4335.2 was added in
2021 to allow DSH evaluators to reevaluate
an individual for competency after they have
been on the waitlist for 60 days.
Implementation of statutory changes may
require funding or other support.
Establishing timeline for court-appointed
evaluators would be dependent upon
increasing the pool of evaluators.
39
M.6
Revise items court-
appointed evaluators must
consider when assessing
competence to include:
• Eligibility for
Diversion
• Likelihood for
restoration
• Medical needs
• Capacity to consent
to medications
• Consideration of
malingering
Statutory
Assists the court in
determining an
individual’s potential
eligibility for
Diversion or whether
another treatment
pathway to
competency
restoration is more
appropriate.
Important to ensure appropriate training,
technical assistance, and quality assurance
measures for court-appointed evaluators are
also implemented in conjunction with this
recommendation, otherwise individuals may
unnecessarily be excluded from Diversion
opportunities.
May also consider whether the court-
appointed evaluator competency assessment
could also include placement
recommendations rather than having a
separate placement performed by the
CONREP Community Program Director.
Would require significant training and
technical assistance on increasing knowledge
of the statewide continuum of placement
options.
M.7
Revise/improve involuntary
medication order statutory
process:
• Involuntary
medication orders
follow the person and
are not specific to the
placement locations.
• Court-appointed
psychologists may
opine on consent
capacity and
potential need for
involuntary
medications when
Statutory
Provides treatment
access and
stabilization for
individuals who do
not have the
capacity to consent
to treatment due to
the current severity
of the symptoms of
their mental illness.
Facilitates improved
care coordination
and rapid re-
stabilization to
prevent
40
providing reports to
the court on
incompetence to
stand trial.
• Remove special
designation
requirements in
Penal code 1369.1
requiring jails to be
designated to provide
involuntary
medications for
felony ISTs and allow
jails to provide
involuntary
medications, when
necessary, ordered
by the court, and
appropriate due
process procedures
have been followed.
rehospitalization in
locked settings
when a justice-
involved individual
decompensates.
M.8
Provide access to
community-based inpatient
treatment, when needed, for
stabilization of acute mental
health symptoms prior to
placement in Diversion
programs.
Funding/
Capacity
Provides increased
mental health
stabilization services
to reduce barriers to
Diversion eligibility
and increase access
to Diversion for
felony ISTs.
The 2021Budget Act includes $250M for DSH
to increase IMD and sub-acute capacity in the
community for felony ISTs, which can be
utilized to provide stabilization services.
M.9
Provide funding to expand
support services to
increasing utilization of
Diversion and community-
Funding/
Operations
Supports providers
in treatment and
support plan
development for
Could pilot these support services in counties
with the greatest number of ISTs to facilitate
greater number of individuals placed in
Diversion.

41
based restoration for felony
ISTs and enhance services
for existing jail-based
competency treatment
programs including:
• Diversion Program
Provider
Support/Technical
Assistance - develop
Diversion technical
assistance/support
teams consisting of
psychiatrists and
criminal justice
experts to provide 24
hours a day 7 days a
week non-urgent and
emergency technical
assistance and
support.
• Forensic Peer
Support Specialists
(or General Peer
Support Specialists)
– Provide funding to
support utilization of
peer support
specialists in the
courts, jails,
Diversion, and
treatment programs.
difficult cases and
responding to
emergent/urgent
Diversion program
and treatment
challenges.
Increases treatment
engagement and
success in
Diversion/communit
y-based treatment
for felony ISTs.
Assists court and
jails with navigation,
identification, and
connection to
system partners to
facilitate
dismissal/Diversion,
case planning, and
effective reentry to
the community.
Expands
opportunities for
higher-risk
individuals to be
served in community
programs.
The 2021 Enacted Budget includes funding to
support probation services for a subset of IST
defendants served in the Los Angeles
community-based restoration program. In
addition, a portion of funding is available to
expand community-based restoration
programs to other counties and can be used
to support probation services.
42
• Probation
Partnerships -
Leverage potential
opportunity for
probation
partnerships to
provide community
Diversion supervision
and rapport building
and increasing client
engagement in
treatment for higher-
risk individuals.
Integration of the
SSI/SSDI Outreach
Access, and
Recovery (SOAR
specialists in
Diversion programs
to increase SSI/SSDI
application success
rates and increase
individual funding for
community-based
housing. Forensic
navigators – provide
funding to support
utilization of liaisons
or navigators in
courts/jails to identify
those who may need
Increases funding
for community-
based housing.
43
community-based
treatment and
supports and make
appropriate
connections with
system partners to
facilitate
dismissal/Diversion,
case planning, and
effective reentry to
the community.
M.1
0
Support individuals with
serious mental illness
remaining stable in the
community by:
• Implementing
Psychiatric Advance
Directives (PADs) -
peers would assist
with the completion
of the PADs (see
above for peer
costs).
• Enhance funding to
the public guardians
to ensure people with
serious mental illness
are appropriately
placed in the
continuum of care.
Policy/
Funding
Reduces
homelessness and
the cycle of
criminalization of
individuals with
serious mental
illness.
Disability Rights California is in the process of
updating their PAD resources and can be a
resource for guidance, forms, etc.
44
M.1
1
Explore alternative jail-
based competency and
community-based
restoration contract models
to maximize utilization of
community facilities for
treatment rather than
providing in-jail competency
treatment.
Policy
Increases
community-based
treatment options
and reduces
reliance on jail-
based treatment to
serve felony ISTs.
Existing authority to expand community-based
restoration programs may be used to support
this contract model.
M.1
2
Expediting assessment and
treatment immediately upon
booking of defendants with
serious mental illness,
including:
• Completing universal
behavioral health and
suicide risk
assessments,
substance abuse
screenings, and
review of records and
behavioral health
history by jail
providers.
• Performing a housing
and service needs
assessment to inform
early consideration of
housing and service
needs for treatment
of ISTs in the
community.
Policy/
Funding
Increases early
access to treatment
and opportunities for
community-based
treatment options.
Additional funding/resources may be needed
by jails, district attorneys, and public
defenders to increase early access to
treatment and increase the number of
behavioral health providers qualified to
perform the assessments and provide
immediate treatment.
45
• Implementing
consideration of the
family perspective
and documentation
of the mental health
history and treatment
of a loved one and
including co-
occurring substance
use disorder
challenges.
• Determine a course
of treatment that may
begin in the jail,
including
medications, and
discharge planning
should start at the
time of booking.
• Early review of cases
at booking or as soon
as possible by
District Attorney and
Public Defender, in
partnership with
county behavioral
health and jail
treatment providers,
for each defendant
screened as
mentally-ill to
46
eliminate those
cases that will not be
filed (defendant to be
released), or for
those defendants in
situations where a
complaint is likely to
be filed, determine if
there are
opportunities for pre-
trial release into
treatment and
services to provide a
recommendation to
the Judge at or
before the time of
arraignment.
M.1
3
Establish requirements
and/or provide
incentives/enhanced rates
to support increased
community-based treatment
and housing for justice-
involved individuals with
SMI, including:
• Increase community
providers, facilities
willing to serve, and
landlords willing to
provide housing for
this population.
Funding/
Statutory
Eliminates barriers
and discriminatory
practices in access
to community-based
treatment for justice-
involved individuals.
Consider utilizing pay for success models.
47
• Increase access to
acute inpatient
services for inmates
under 5150s.
M.1
4
Provide flexibilities, and
expedited licensing to
increase access to inpatient
beds and housing,
including:
• Expedited licensing
of Psychiatric Health
Facilities (PHFs) and
Mental Health
Rehabilitation
Centers (MHRCs).
• Streamlining/coordin
ation of licensing
bodies when trying to
establish new adult
residential facilities
and other treatment
facilities.
Policy
Facilitates faster
expansion of
community
treatment and
housing resources.
Eliminates
perceived licensing
barriers to quick
expansion of
treatment/housing
resources.
M.1
5
Revise DSH’s CONREP
Community Program
Director Role, placement
criteria, and assessment
process to facilitate
increased felony IST
placement to CONREP,
community-based
restoration and Diversion
programs and increased
transitions from state
Statutory
Increases access to
Diversion and
community-based
restoration
programs for felony
ISTs.
Increases state
hospital capacity for
ISTs with highest
level of treatment
48
hospitals to the CONREP
community treatment
continuum for individuals
committed to DSH as Not
Guilty by Reason of Insanity
or Offenders with Mental
Health Disorders.
needs by stepping
down individuals
from state hospitals
to CONREP
continuum.
M.1
6
Allow access to and
regularly assess eligibility
for transition to DSH funded
Diversion opportunities for
individuals who are treated
at DSH hospitals and jail-
based competency
treatment programs.
Policy/
Funding
Provides pathway to
community
treatment and
supports reduction
in recidivism for
individuals who
have received
restoration of
competency
treatment in a DSH
hospital or JBCT
program.
M.1
7
Provide increased and
ongoing funding to support
expansion of DSH Diversion
and community-based
restoration programs.
Funding
Provides increased
access to
community-based
treatment options.
Existing funding and expansion funding
contained in the 2021-22 Budget Act for DSH
Diversion programs is one-time funding.
Currently community-based restoration
programs are only operated in partnership
with Los Angeles County. The 2021-22
Budget Act provides funding for 552 additional
beds to expand the existing program and
develop new community-based restoration
programs in other counties across three fiscal
years.

49
Support for housing and infrastructure needs
when establishing new programs should be
considered.
50
Long-Term Strategies: Solutions that can begin implementation by January 10, 2024 and January 10, 2025
Goals:
a. Break the cycle of criminalization.
b. Reduce the number of individuals found incompetent to stand trial on felony charges.
c. Provide bridge funding or strategies until broader behavioral health transformation initiatives are fully implemented
including CalAIM, Behavioral Health Care Continuum Expansion, and Community Care Expansions.
#
Strategy
Type
Potential Impact
Other Considerations
L.1
Partner with the Homeless
Coordinating and Financing
Council (now the California
Interagency Council on
Homelessness) to:
• Advocate to HUD to
include the definition
of at-risk of
homelessness as
and eligible
population for
resources.
• Advocate with HUD
to leverage existing
allocations from
federal government
to local Continuums
of Care (CoCs).
• Consider flexibilities
around housing first
approaches and
ensure definition of
homelessness
Policy
Increased
coordination and
access to housing
resources for
individuals with
serious mental
illness to eliminate
cycling in and out of
homelessness.

51
includes at-risk of
homelessness
populations.
• Provide training and
technical assistance
to CoCs, Criminal
Justice, and
Behavioral Health
partners on how to
provide effective
housing services to
this population.
• Explore and support
strategies to
exchange data to
ensure that the
Behavioral
Health/Criminal
Justice population is
included in CoC
resourced efforts.
The Criminal Justice
system needs to be
connected to the
homeless crisis
response system.
• Encourage local
housing system
leaders to participate
in existing
interdisciplinary
meetings focused on
52
justice-involved
populations.
• Support inclusion of
individuals with
serious mental illness
and justice
involvement in
housing priorities/
preferences for
housing funding.
L.2
Support effective
implementation of the
proposed Cal-AIM
(California Advancing &
Innovating Medi-Cal)
components that impact the
justice involved, including:
• Enrollment in Medi-
Cal prior to release.
• 90-day in-reach to
stabilize health and
wellness, provide
warm hand-offs and
prepare for
community
reintegration.
• Intensive community-
based care and
coordination –
enhanced care
management (ECM).
• Access to community
support (food and
Funding/
Policy
Provides
coordination of
medical, behavioral
health, and non-
clinical social
services for justice-
involved individuals
prior to and upon
release from county
jails. Access to
services upon
release from jail can
help reduce the
cycle of
criminalization for
individuals with
serious mental
illness.
Department of Health Care Services (DHCS)
has submitted application for Medi-Cal waiver
to the Centers for Medicare and Medicaid
Services for approval.
While overall implementation is a longer-term
strategy, planning for implementation is
occurring with stakeholders in the short and
medium-term.
53
housing) post
release.
• Capacity building for
workforce, IT/data
systems,
infrastructure.
• Seek the IMD
exclusion waiver.
L.3
Develop quality
improvement oversight/peer
review of court-appointed
evaluators and their reports,
which may include:
• Developing a
certification program.
• Implementing pay for
performance
strategies to tie
funding to quality.
• Requiring
standardized training.
• Implementing a peer
review process to
improve quality of
reports.
Funding/
Statutory
Increased quality
and timing of court-
appointed evaluator
reports. Reduced
time in jail for
individuals pending
competency
assessments. May
reduce the number
of individuals found
incompetent to
stand trial due to
poor quality reports.
Consideration should be given to whether a
certification, quality improvement, and
oversight program should be implemented at
the state level, by the Judicial Council or by a
private/other certification program provider.
Increased funding for court-appointed
evaluator pay (strategy M.4) could be linked
to quality improvement strategies. Individuals
participating in quality improvement
efforts/training or who are certified are eligible
to receive higher pay for evaluations.
L.4
Increase opportunities for
alternatives to arrest and
pre-booking Diversion,
including:
• Mobile/non-police
crisis response
teams.
Funding
Reduces
incarceration and
increases access to
community-based
treatment for
individuals with
serious mental
illnesses.
There may be opportunities to leverage
resources with court pre-trial programs.
While overall implementation is a longer-term
strategy, planning for implementation with
stakeholders would be in the short and
medium-term.
54
• Sobering or triage
centers.
• Diversion centers
including Federally
Qualified Health
Center models.
L.5
Expand community
treatment and housing
options for individuals living
with serious mental illness
and who are justice-
involved, including:
• Provide dedicated
funding to develop
housing to support
Diversion and
community-based
restoration.
• Provide funding to
incentivize the
development and
expansion of
community-based
restoration programs
across the state.
• Provide incentives or
flexible housing pool
models for housing
developers, providers
of supportive housing
(including peer-run
organizations), and
owners of rental units
Funding/
Policy
Increases access to
Diversion and
community-based
treatment for felony
ISTs. Provides
treatment and
housing options to
provide community-
based treatment and
Diversion.
Supports
infrastructure
development and
prioritization for
justice-involved
individuals including
felony ISTs.
55
to create additional
housing resources or
provide operating
subsidies or supports
for justice-involved
individuals with
serious mental
illnesses.
• Include justice-
involved individuals
with serious mental
illness as priorities in
homelessness,
behavioral health,
and community care
infrastructure
expansion funding.
• Provide landlord
incentives.
• Expand Social
Rehabilitation
facilities.
• Develop unlocked
residential housing
with treatment and
supports.
• Support regional
programs and
approaches for
behavioral health and
housing strategies,
especially in less
56
densely populated
regions.
• Increase permanent
supportive housing
opportunities for
justice-involved
individuals with
serious mental
illnesses.
• Consider funding
support for
Accessory Dwelling
Units (ADU)
development to
support families’
ability to provide
independent housing
for loved ones with
SMI on their
properties.
L.6
Develop new licensing
category for enriched and
intensive community
treatment options for
individuals living with
Serious Mental Illness
including individuals who
are justice-involved which
may include provisions of
mental health, health care,
and intensive support
services in a home-like
setting:
Statutory
Increases intensive
community-based
treatment options for
individuals with
serious mental
illnesses to prevent
homelessness and
criminalization.
57
• Explore similar model
to the Short-term
Residential
Therapeutic
Programs models
that serve children
and youth whose
needs create barriers
to placement in
family-based care.
• Explore similar
licensing categories
to those that support
adults with
developmental
disabilities.
L.7
Facilitate appropriate
information sharing and
support cross-system data
initiatives across State,
courts, and local entities
that serve ISTs.
• Develop State Health
Information Guidance
on sharing health
and housing
information in the
context of serving
people involved in
the criminal justice
systems, including
the development of
standard
Policy
Facilitates improved
treatment/coordinati
on. Supports
research,
evaluation, and
policy development
to inform ongoing
strategies and
investments.
58
authorizations for
release of
information and
MOU’s and provide
training and technical
assistance on
guidance
implementation.
• Provide funding to
support counties to
undertake analyses
of their criminal
justice populations,
including those with
behavioral health
needs to understand
trends and identify
data-driven
strategies to reduce
the number of ISTs.
• Provide funding to
develop a state
approach to monitor
key data at the
intersection of
criminal justice,
behavioral health,
and homelessness.
L.8
Support the development
and expansion of a
culturally and linguistically
competent workforce to
meet an individual’s forensic
Funding/
Policy
Provides a diverse
workforce trained to
provide services and
support to justice-
involved individuals
59
and behavioral health
needs, including:
• Funding for forensic
fellowships.
• Utilizing 4
th
year
residents and
psychology students
to provide court-
appointed
evaluations.
• Support increased
psychologist
education and
training and
psychiatric residency
programs with
rotation requirements
to serve justice-
involved individuals.
• Explore expansion of
mental health and
other professionals to
serve justice-involved
individuals.
• Expand the use of
peer support
specialists and family
members.
• Support care team
models so individuals
are working at the
top of their licensure.
with serious mental
illness.
60
• Provide recruitment
and retention
incentives.
• Identify funding
streams that could be
braided (and
augmented) to
address workforce
shortages.
• Educate workforce
on serving in the role
of the housing
advocate,
collaborative justice
principles,
motivational
interviewing,
assessing and
mitigating
dangerousness,
implicit bias, and
other culturally
relevant
competencies.
L.9
Phase out the reliance and
utilization of jail-based
competency treatment
programs as community-
based treatment and
Diversion program options
for felony ISTs are
expanded.
Policy
Prioritizes
community-based
treatment options for
individuals with
serious mental
illness to provide for
improved outcomes
and connection to
long-term
61
community
treatment and
supports.
L.10
Explore and, if needed,
implement improvements to
policies and practices
governed by the Mental
Health Services Act and the
Lanterman-Petris-Short Act
to facilitate access to care
and treatment for individuals
who are experiencing
severe and disabling mental
health crisis.
Statutory
Increased access to
treatment and
reduced criminal-
justice involvement
for individuals with
serious mental
illness.
L.11
Provide funding support to
counties to expand access
to AB1810 Mental Health
Diversion (Penal Code
1001.36), including for
misdemeanors.
Funding/
Policy
Increasing access to
mental health
Diversion
opportunities for
misdemeanors can
reduce the cycle of
incarceration at an
earlier stage
reducing the
potential for future
felony arrest and
IST determination.
Consider eliminating county matching
requirements which can create barriers to MH
Diversion expansion.
Include funding for housing individuals
participating in Mental Health Diversion
L.12
Provide increased access to
permanent supportive
housing for individuals with
serious mental illness who
are justice-involved.
Funding/
Policy
Individuals found
incompetent to
stand trial on Felony
charges and
referred to DSH are
often unsheltered

62
homeless at the
time of arrest and
have had multiple
prior criminal justice
encounters.
Providing
permanent
supportive housing
will help reduce the
cycle of
criminalization for
individuals with
serious mental
illness.
L.13
Revise incompetent to
stand trial statutes to
require the prosecution to
establish competency,
rather than current
requirement of the defense
to establish incompetency.
Statutory
Streamlines
pathway to
treatment for
individuals with
serious mental
illness where there
is clear evidence of
incompetence.
[1]
Incompetent to Stand Trial Solutions Workgroup Website: https://www.chhs.ca.gov/home/committees/ist-solutions-workgroup/
https://www.chhs.ca.gov/home/committees/ist-solutions-workgroup/

63
Appendix A: IST Solutions Working Group Membership and Affiliations
Working Group 1: Early Access to Treatment and Stabilization for Individuals
Found Felony IST
• Co-Chair: Melanie Scott, PsyD, Assistant Chief Psychologist, California
Department of State Hospitals
• Co-Chair: Katherine Warburton, DO, Medical Director, Deputy Director of
Clinical Operations, California Department of State Hospitals
• Deanna Adams, Senior Analyst, Judicial Council of California
• Kirsten Barlow, National Alliance of Mental Illness (NAMI) – California
• Francine Byrne, Principal Manager, Criminal Justice Services, Operations &
Programs Division, Judicial Council of California
• Elise Devecchio-Cavagnaro, Ph.D., Consulting Psychologist, Department of
Health Care Services
• Brenda Grealish, Executive Officer, Council on Criminal Justice and Behavioral
Health (CCJBH), California Department of Corrections and Rehabilitation
(CDCR) Office of the Secretary
• Paige Hoffman, Staff Services Analyst, Council on Criminal Justice and
Behavioral Health, California Department of Corrections and Rehabilitation
• Karen Larsen, Health & Human Services Agency Director, Yolo County &
County Behavioral Health Directors Association (CBHDA)
• Kristopher Kent, Attorney, California Department of State Hospitals
• Farrah McDaid Ting, Senior Legislative Representative, Administration of
Justice, California State Association of Counties (CSAC)
• Stephen Manley, Superior Court Judge, Santa Clara County
• Christy Mulkerin, MD, Chief Medical Officer, San Luis Obispo County Jail
• Kim Pederson, Senior Attorney, Disability Rights California
• Dawn Percy, Deputy Director, Department of Developmental Services
• Jonathan Raven, Chief Deputy District Attorney, Yolo County (CDAA)
• Stephanie Regular, Assistant Public Defender, Contra Costa County Public
Defender Office & Co-Chair of the Mental Health Committee of the California
Public Defender Association (CPDA)
• Marni Sager, Manager, Department of Developmental Services
• Cory Salzillo, Legislative Director, California State Sherrif’s Association
Working Group 2: Diversion and Community-Based Restoration for Felony ISTs
• Co-Chair: Katherine Warburton, DO, Medical Director, Deputy Director of
Clinical Operations, California Department of State Hospitals
• Co-Chair: Stephanie Welch, Deputy Secretary of Behavioral Health, California
Health and Human Services Agency
64
• Francine Byrne, Principal Manager, Criminal Justice Services, Operations &
Programs Division, Judicial Council of California
• Jessica Cruz, MPA/HS, CEO, National Alliance of Mental Illness (NAMI) –
California
• Steven Kite, COO, National Alliance of Mental Illness (NAMI) – California
• Sarah Desmarais, PhD, Senior Vice President, Policy Research Associates, Inc.
• Elise Devecchio-Cavagnaro, Ph.D., Consulting Psychologist, Department of
Health Care Services
• Anita Fisher, Council on Criminal Justice and Behavioral Health / Family
Member
• Neil Gowensmith, Ph.D. Assistant Professor, University of Denver, Licensed
Clinical & Forensic Psychologist
• Brenda Grealish, Executive Officer, Council on Criminal Justice and Behavioral
Health (CCJBH), California Department of Corrections and Rehabilitation
(CDCR) Office of the Secretary
• Cathy Hickenbotham, Council on Criminal Justice and Behavioral Health
(CCJBH), California Department of Corrections and Rehabilitation (CDCR)
• Scarlet Hughes, Executive Director, California Association of Public
Administrators, Public Guardians and Public Conservators (CAPAPGPC)
• Tony Hobson, PhD, Behavioral Health Director, Plumas County
• John Keene, Chief Probation Officer, San Mateo County & President-Elect,
Chief Probation Officers of California CPOC)
• Veronica Kelley, Director, San Bernardino County Department of Behavioral
Health & Board President, California Behavioral Health Directors Association
(CBHDA)
• Michelle Cabrera, Executive Director, California Behavioral Health Directors
Association (CBHDA)
• Kristopher Kent, Attorney, California Department of State Hospitals
• Pamila Lew, Senior Attorney, Disability Rights California (DRC)
• LD Louis, Assistant District Attorney, Alameda County District Attorneys Office &
California District Attorneys Association (CDAA)
• Farrah McDaid Ting, Senior Legislative Representative, Administration of
Justice, California State Association of Counties (CSAC)
• Dawn Percy, Deputy Director, Department of Developmental Services
• Jonathan Raven, Chief Deputy District Attorney, Yolo County (CDAA)
• Marni Sager, Manager, Department of Developmental Services
• Gilda Valeros, Supervising Attorney for Santa Clara County’s Public Defender’s
Office
• Stephen Manley, Superior Court Judge, Santa Clara County

65
Working Group 3: Initial County Competency Evaluations
• Co-Chair: Charles Scott, MD, Chief, Division of Psychiatry and the Law,
Forensic Psychiatry Training Director, and Professor of Clinical Psychiatry at the
University of California, Davis Medical Center
• Co-Chair: Katherine Warburton, DO, Medical Director, Deputy Director of
Clinical Operations, California Department of State Hospitals
• Deanna Adams, Senior Analyst, Judicial Council of California
• Francine Byrne, Principal Manager, Criminal Justice Services, Operations &
Programs Division, Judicial Council of California
• Katherine Clark, Assistant Program Budget Manager, California Department of
Finance
• Matthew Greco, Deputy District Attorney, San Diego County District Attorney's
Office
• Scarlet Hughes, Executive Director, California Association of Public
Administrators, Public Guardians and Public Conservators (CAPAPGPC)
• Stephen Manley, Superior Court Judge, Santa Clara County
• Farrah McDaid Ting, Senior Legislative Representative, Administration of
Justice, California State Association of Counties (CSAC)
• Danny Offer, National Alliance of Mental Illness (NAMI) – California
• Ira Packer, PhD, Clinical Professor of Psychiatry & Director, Forensic
Psychology Residency, University of Massachusetts Medical School
• Neil Gowensmith, Ph.D. Assistant Professor, University of Denver, Licensed
Clinical & Forensic Psychologist
• Dawn Percy, Deputy Director, Department of Developmental Services
• Jonathan Raven, Chief Deputy District Attorney, Yolo County (CDAA)
• Stephanie Regular, Assistant Public Defender, Contra Costa County Public
Defender Office & Co-Chair of the Mental Health Committee of the California
Public Defender Association (CPDA)
• Marni Sager, Manager, Department of Developmental Services
• Todd Schirmer, PhD, CCHP, Forensic Division Director, Marin County
Behavioral Health & Recovery Services & County Behavioral Health Directors
Association (CBHDA)
